
AI Compliance in Pharma: Regulatory Risks, Monitoring Frameworks, and Governance Models
Prevent risky AI outputs before they ship. Set up continuous compliance monitoring with guardrails, audit trails, and real-time exception handling.

A Patient Support Program (PSP) is a structured suite of services developed to assist patients at every stage of their treatment journey—from initial prescription to long-term adherence. These services typically cover medication access, reimbursement support, disease education, digital engagement, lifestyle coaching, and more.
For pharmaceutical companies, PSPs have become essential tools to optimize real-world evidence (RWE), ensure medication adherence, and improve patient experience, which in turn contributes to stronger outcomes and brand loyalty. PSPs also support regulatory and commercial objectives by capturing valuable data and ensuring proper use of high-cost therapies.
For digital health startups and platforms, PSPs offer a scalable frontier to deploy modular, patient-centric solutions that integrate into broader care ecosystems. These programs are fertile ground for innovation around automation, engagement, and personalization.
The value of PSPs extends beyond patient satisfaction or brand goodwill. They directly address operational and clinical inefficiencies by:
Simply put, a well-designed PSP can influence both the top and bottom line for pharmaceutical brands.
While the structure of PSPs varies by product type and patient population, successful programs tend to include the following pillars:
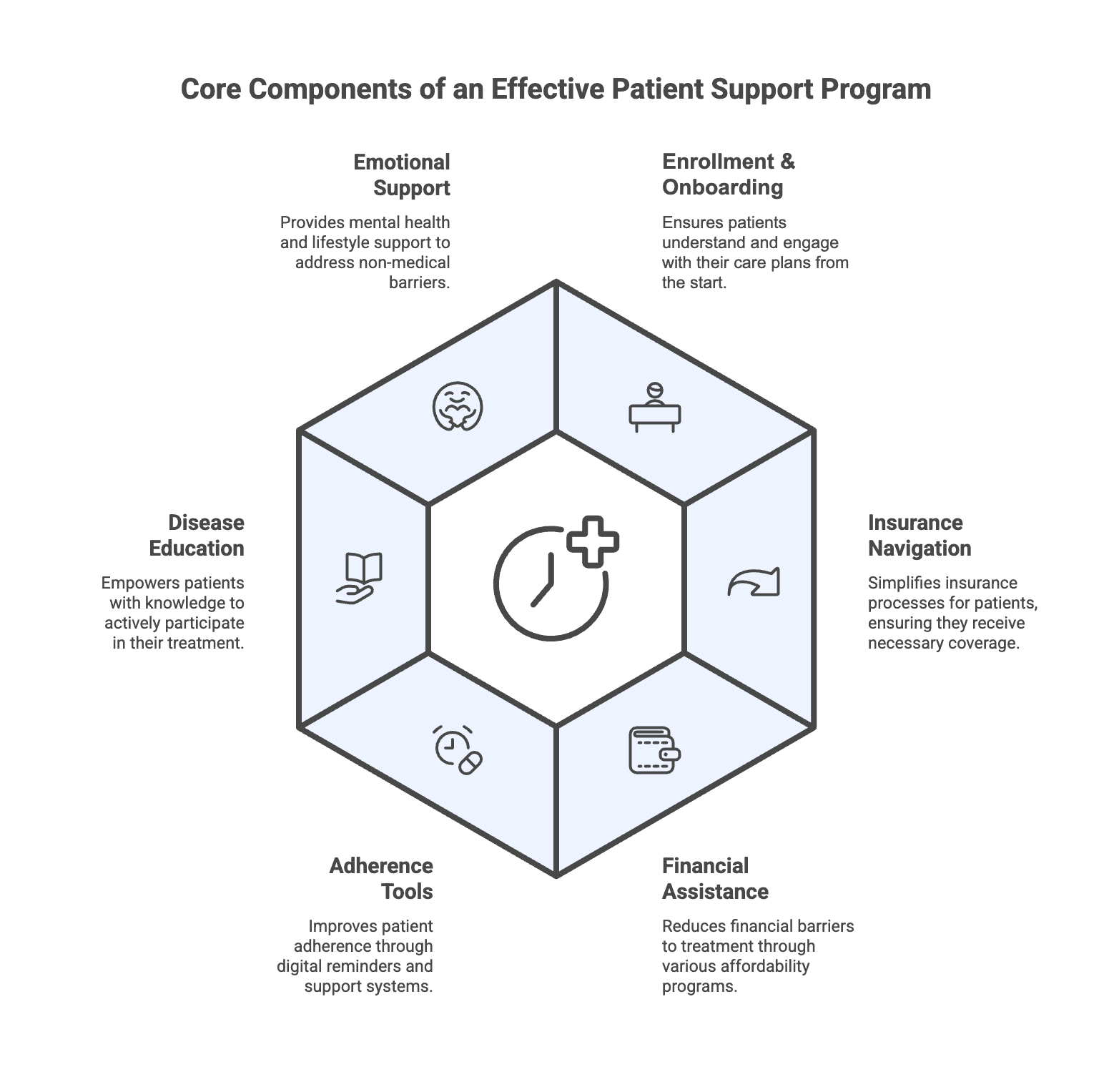
Support services to help patients complete enrollment forms, obtain prior authorizations, and understand their care plans. Early engagement ensures that patients don’t abandon treatment before it even begins.
Many patients are unfamiliar with insurance workflows. PSPs simplify this through dedicated teams or automated tools that manage prior authorizations, benefits verification, appeals processes, and co-pay eligibility.
High out-of-pocket costs are a leading cause of non-initiation. PSPs often include co-pay cards, patient assistance programs (PAPs), or connections to financial foundations to reduce cost-related abandonment.
Digital nudges, medication reminders, refill tracking, and live nurse support can drastically improve adherence. Some PSPs use AI or predictive analytics to flag patients at risk of drop-off.
Many patients drop out simply due to fear or misunderstanding. Educational content—via SMS, email, apps, or HCP outreach—helps patients and caregivers become active participants in treatment.
PSPs that include mental health coaching, social support, or lifestyle planning (diet, mobility, sleep) address non-medical barriers to success. This humanized layer increases trust and satisfaction.
Traditional PSPs were often fragmented, heavily reliant on call centers, and difficult to scale. Today, digital health innovators are reimagining PSPs through platform-based approaches:
This shift toward digital-first PSPs improves scalability, cost-effectiveness, and patient satisfaction while enabling better data collection and personalization.
No two therapies or patient populations are the same. That’s why successful PSPs require intentional design that aligns with:
Pharma companies must avoid over-engineered, one-size-fits-all programs and instead prioritize modularity and patient segmentation.
As healthcare moves steadily toward value-based care models, where success is measured by patient outcomes rather than volume, PSPs will become even more vital.
Expect increased convergence of PSPs with digital therapeutics, remote patient monitoring, and AI-driven care coordination in the next wave.
Patient Support Programs have evolved from back-office support services into mission-critical engines for patient experience, adherence, and brand differentiation. In a crowded therapeutic market with rising pressure on real-world outcomes, PSPs are now central to pharma’s commercial success and digital health's platform opportunities.
Organizations that treat PSPs as strategic assets, rather than compliance checkboxes will be best positioned to lead in the next era of connected, patient-centric care.
Want to explore how Zelthy can transform your PSP operations? Book a demo. Contact us at connect@zelthy.com or send us a DM on LinkedIn for more information.
Dive into our comprehensive collection of blogs covering diverse topics in project management and beyond.
Reach out to us for inquiries, support, or partnership opportunities. We're here to assist you!
Use our convenient contact form to reach out with questions, feedback, or collaboration inquiries.